PURPOSE:
Dose verification in preclinical radiotherapy is often challenged by a lack of standardization in the techniques and technologies commonly employed along with the inherent difficulty of dosimetry associated with small-field kilovoltage sources. As a consequence, the accuracy of dosimetry in radiobiological research has been called into question. Fortunately, the development and characterization of realistic small-animal phantoms has emerged as an effective and accessible means of improving dosimetric accuracy and precision in this context. The application of three-dimensional (3D) printing, in particular, has enabled substantial improvements in the conformity of representative phantoms with respect to the small animals they are modeled after. In this study, our goal was to evaluate a fully 3D printed mouse phantom for use in preclinical treatment verification of sophisticated therapies for various anatomical targets of therapeutic interest.
METHODS:
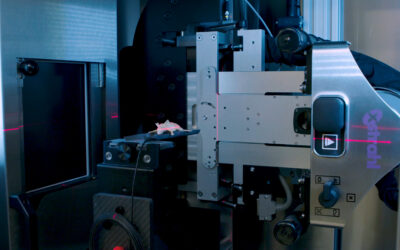
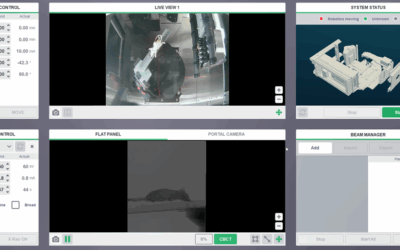
An anatomically realistic mouse phantom was 3D printed based on segmented microCT data of a tumor-bearing mouse. The phantom was modified to accommodate both laser-cut EBT3 radiochromic film within the mouse thorax and a plastic scintillator dosimeter (PSD), which may be placed within the brain, abdomen, or 1-cm flank subcutaneous tumor. Various treatments were delivered on an image-guided small-animal irradiator in order to determine the doses to isocenter using a PSD and validate lateral- and depth-dose distributions using film dosimeters. On-board cone-beam CT imaging was used to localize isocenter to the film plane or PSD active element prior to irradiation. The PSD irradiations comprised a 3 × 3 mm2 brain arc, 5 × 5 mm2 parallel-opposed pair (POP), and 5-beam 10 × 10 mm2 abdominal coplanar arrangement while two-dimensional (2D) film dose distributions were acquired using a 3 × 3 mm2 arc and both 5 × 5 and 10 × 10 mm2 3-beam coplanar plans. A validated Monte Carlo (MC) model of the source was used as to verify the accuracy of the film and PSD dose measurements. computer-aided design (CAD) geometries for the mouse phantom and dosimeters were imported directly into the MC code to allow for highly accurate reproduction of the physical experiment conditions. Experimental and MC-derived film data were co-registered and film dose profiles were compared for points above 90% of the dose maximum. Point dose measurements obtained with the PSD were similarly compared for each of the candidate (brain, abdomen, and tumor) treatment sites.
RESULTS:
For each treatment configuration and anatomical target, the MC-calculated and measured doses met the proposed 5% agreement goal for dose accuracy in radiobiology experiments. The 2D film and MC dose distributions were successfully registered and mean doses for lateral profiles were found to agree to within 2.3% in all cases. Isocentric point-dose measurements taken with the PSD were similarly consistent, with a maximum percentage deviation of 3.2%.
CONCLUSIONS:
Our study confirms the utility of 3D printed phantom design in providing accurate dose estimates for a variety of preclinical treatment paradigms. As a tool for pretreatment dose verification, the phantom may be of particular interest to researchers for its ability to facilitate precise dosimetry while fostering a reduction in cost for radiobiology experiments.
Esplen N, Therriault-Proulx F, Beaulieu L, Bazalova-Carter M.