Publication/Study:
Autophagy Regulation of Metabolism Is Required for CD8+ T Cell Anti-tumor Immunity
Authors:
DeVorkin L, Pavey N, Carleton G, Comber A, et al
Key Findings:
While autophagy is a necessary process to ensure appropriate infection response in cells, researchers in this study sought to better understand how alterations in the autophagy process might affect or regulate anti-tumor immunity.
The study’s results demonstrate that mice that lacking the autophagy genes Atg5, Atg14, orAtg16L1 “display a dramatic impairment in the growth of syngeneic tumors.” Equally important is the finding that the T cells without Atg5 subsequently experience “a profound shift to an effector memory phenotype and produce greater amounts of interferon-γ (IFN-γ) and tumor necrosis factor α (TNF-α).” At a more detailed level, CD8+ T cells deficient in the Atg5 autophagy gene also show changes in glucose metabolism that, while potentially affecting the anti-tumor progress of the autophagy alteration, can be controlled through glucose restriction. The bottom line, according to researchers, is that “autophagy-dependent changes in CD8+ T cell metabolism directly regulate anti-tumor immunity.”
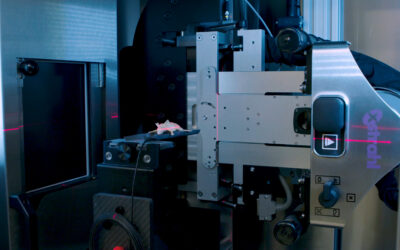
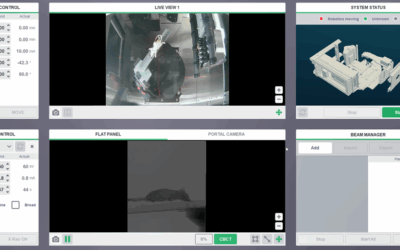
The Value of SARRP:
In this study, SARRP played an important role in assisting with the generation of the Bone Marrow Chimeric (BMC) mice necessary to test the role played by Atg5-depleted cells in inhibiting tumor growth. SARRP provided researchers with a viable instrument for successfully irradiating existing bone marrow and ensuring the transplantation of both the variable (Atg-/-) and control (Atg+/-) marrow. As the study is intended to further valuable research behind potential human cancer treatments, it was imperative that researchers could replicate actual clinical environments as closely as possible while delivering specifically targeted radiation to their mice.