Combined immune checkpoint blockade has led to rare autoimmune complications, such as fatal myocarditis. Recent approvals of several anti-programmed death 1 (anti-PD-1) drugs for lung cancer treatment prompted ongoing clinical trials that directly combine PD-1 inhibitors with thoracic radiotherapy for locally advanced lung cancer. Overlapping toxicities from either modality have the potential to increase the risk for radiation-induced cardiotoxicity (RICT), which is well documented among patients with Hodgkin’s disease and breast cancer.
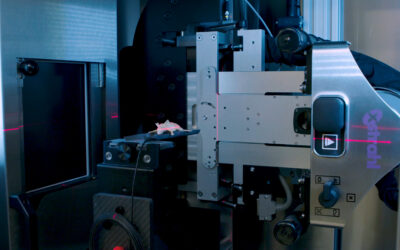
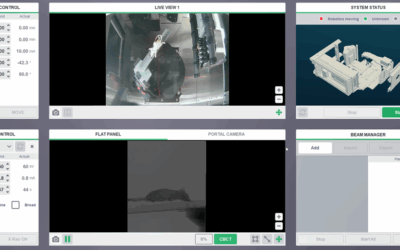
To investigate cardiotoxicity without the compounding pulmonary toxicity from thoracic radiotherapy, Du S, Zhou L, et al, in their study “PD-1 Modulates Radiation-Induced Cardiac Toxicity through Cytotoxic T Lymphocytes” developed a technique to deliver cardiac irradiation (CIR) in a mouse model concurrently with PD-1 blockade to determine the presence of cardiac toxicity by using physiological testing and mortality as end points along with histological analysis, on an Xstrahl Small Animal Radiation Research Platform (SARRP).
They observed an acute mortality of 30% within 2 weeks after CIR plus anti-PD-1 antibody compared with 0% from CIR plus immunoglobulin G (p = 0.023). Physiological testing demonstrated a reduced left ventricular ejection fraction (p < 0.01) by echocardiogram. Tissue analyses revealed increased immune cell infiltrates within cardiac tissue. Depletion of CD8-positive lymphocytes with anti-CD8 antibody reversed the acute mortality, suggesting that the toxicity is CD8-positive cell-mediated. To validate these findings using a clinically relevant fractionated radiotherapy regimen, they repeated the study by delivering five daily fractions of 6 Gy. Similar mortality, cardiac dysfunction, and histological changes were observed in mice receiving fractionated radiotherapy with concurrent anti-PD-1 therapy.
This study provides strong preclinical evidence that radiation-induced cardiotoxicity is modulated by the PD-1 axis and that PD-1 blockade should be administered with careful radiotherapy planning with an effort of reducing cardiac dose.
This Xstrahl In Action was adapted from a article found on a National Library of Medicine website.