There have been a growing number of studies combining radiotherapy with immunotherapy to enhance both local and metastatic tumor cell kill leveraging the immune-mediated abscopal effect. This abscopal effect can enable the killing of metastatic cells, distant from the irradiated site. However, clinical trials show limited treatment benefit for lung tumors with abscopal response rates remaining low due to immunosuppression.
In the paper “Priming the Abscopal Effect Using Multifunctional Smart Radiotherapy Biomaterials Loaded with Immunoadjuvants” Michele Moreau, Sayeda Yasmin-Karim, Sijumon Kunjachan, Neeharika Sinha, Felix Gremse, Rajiv Kumar, Kwok Fan Chow, and Wilfred Ngwa, investigate the use of multifunctional smart radiotherapy biomaterials (SRBs) loaded with immunoadjuvants for boosting the abscopal effect of local radiotherapy.
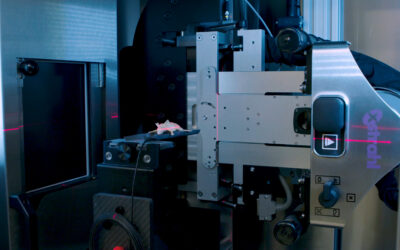
SRBs were designed similarly to currently used inert radiotherapy biomaterials, incorporating a biodegradable polymer with reservoir for loading payloads of the immunoadjuvant anti-CD40 monoclonal antibody. Lung (LLC1) tumors were generated both on the right and left flank of each mouse, with the left tumor representing metastasis. The mice were randomized and divided into eight cohorts with four cohorts receiving image-guided radiotherapy at 5 Gy and another similar four cohorts at 0 Gy. Image-guided radiotherapy and Computed Tomography (CT) imaging were performed using the Xstrahl Small Animal Radiation Research Platform (SARRP). Tumor volume measurements for both flank tumors and animal survival were then assessed over 25 weeks.
Tumor volume measurements showed significantly enhanced inhibition in growth for the right flank tumors of mice in the cohort treated with SRBs loaded with CD40 mAbs and image-guided radiotherapy. Results also suggest that the use of polymeric SRBs with CD40 mAbs without radiotherapy could generate an immune response, consistent with previous studies showing such response when using anti-CD40. Overall, 60% of mice treated with SRBs showed complete tumor regression during the observation period, compared to 10% for cohorts administered with anti-CD40 mAbs, but no SRB. Complete tumor regression was not observed in any other cohorts.
It was concluded that the findings of this paper justify more studies varying radiotherapy doses and quantifying the immune-cell populations involved when using SRBs. Such SRBs could be developed to replace currently used radiotherapy biomaterials, allowing not only for geometric accuracy during radiotherapy, but also for extending radiotherapy to the treatment of metastatic lesions.
This Xstrahl In Action was adapted from a article found on a National Library of Medicine website.